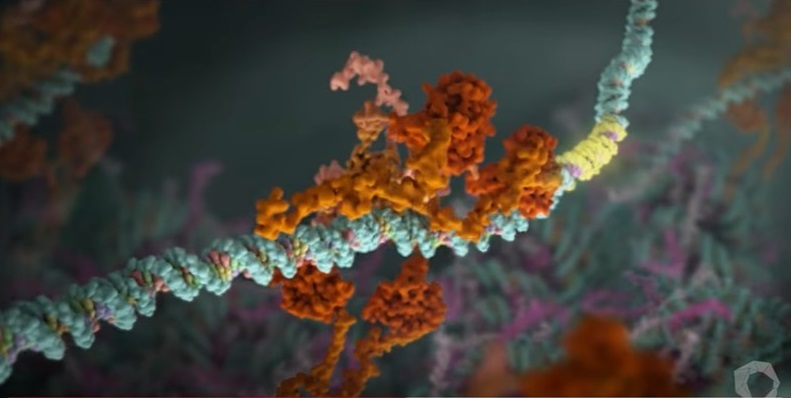
The p53 protein, often referred to as the “guardian of the genome,” plays a crucial role in cell biology by regulating cell cycle, apoptosis, and genomic stability. Its functions include activating DNA repair proteins, arresting cell growth in response to DNA damage, initiating programmed cell death, and contributing to the senescence response. Alterations of p53 are present in more than half of all human cancers, collectively making them the most common event in the development of cancer.
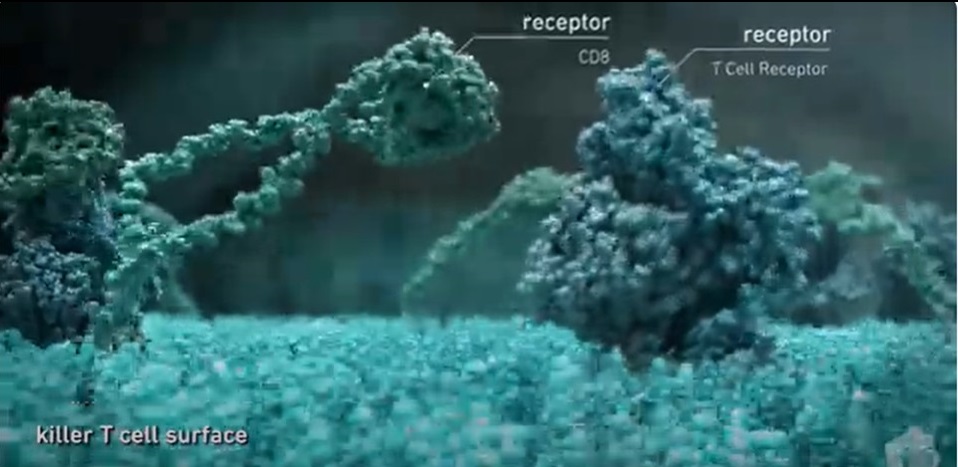
Chimeric antigen receptor (CAR) T cell therapy is a groundbreaking approach that engineers T cells to target specific antigens on cancer cells. In this context, researchers led by Carl June, MD, at the Perelman School of Medicine, University of Pennsylvania, investigated the potential of modulating the p53 signaling network with Δ133p53α to enhance CAR T cell therapy’s effectiveness in their article published in The Proceedings of the National Academy of Sciences and titled, “Enhancing chimeric antigen receptor T cell therapy by modulating the p53 signaling network with Δ133p53α.”
Increased antitumor function of CAR T cells
June and colleagues focused on Δ133p53α, a variant of the p53 protein whose expression decreases with age in human T cells. Their study demonstrated that continuous expression of Δ133p53α significantly improved the antitumor function of CAR T cells. This enhancement was observed in CAR T cells derived from both healthy donors and individuals with chronic lymphocytic leukemia (CLL) who had previously failed to respond to CAR T cell therapy during clinical trials. By expressing Δ133p53α, CAR T cells exhibited improved metabolic function, resulting in enhanced antitumor activity, particularly under conditions of high tumor burden. Even in nutrient-limiting environments, CAR T cells expressing Δ133p53α showed increased proliferation and effectively cleared more tumor cells due to enhanced biosynthetic processes and improved mitochondrial function.
According to the researchers, “CAR T cell therapy, a transformative treatment for blood cancers, is limited by T cell dysfunction, especially in chronic lymphocytic leukemia (CLL). Our study reveals a pivotal role for the human and great ape-specific p53 isoform, Δ133p53α, in enhancing the therapeutic efficacy of CAR T cells. Expressing Δ133p53α in CAR T cells improves their metabolic robustness, enabling superior antitumor function, particularly under high tumor burden conditions.”
Conclusions
The findings of this study highlight the significance of the p53 signaling network in regulating prolonged CAR T cell responses and offer insights into developing improved cancer therapies utilizing T cells. The researchers believe that Δ133p53α could be a promising target for enhancing CAR T cell therapy’s effectiveness, not only in CLL but also in solid tumor indications. They concluded, “In summary, our findings point to the potential for using the p53 isoform Δ133p53α to improve CAR T cell antitumor function through the modulation of the p53 signaling network. Constitutive expression of Δ133p53α may represent a viable translational strategy for improving CAR T cell therapy in CLL and in solid tumor indication and warrants further investigation.”
In conclusion, the study identifies a concrete possibility to enhance the effectiveness of CAR-T cell therapy by modulating the expression of Δ133p53α, offering hope for the development of better treatments for cancer patients in the future.

Leave a Reply