Antibiotic resistance, one of the gravest challenges in modern medicine, continues to undermine our ability to treat bacterial infections effectively. With bacteria developing resistance to previously potent drugs, scientists are racing to find innovative strategies to counteract this growing crisis. One recent breakthrough focuses on an unexpected yet vital factor in bacterial survival: their dependence on zinc.
The Role of Zinc in Bacterial Survival
Zinc is a crucial trace element for bacteria, playing a key role in enzyme activity, gene expression, and cellular integrity. Resistant bacteria, such as those producing metallo-β-lactamases, rely heavily on zinc for their survival and resistance mechanisms. Metallo-β-lactamases, in particular, are enzymes that render β-lactam antibiotics—like carbapenems—ineffective by breaking down their molecular structure. These enzymes, however, are only functional in the presence of zinc. This dependency has become the focal point of new research aimed at disarming resistant bacteria.
Targeting Zinc: A New Frontier in Research
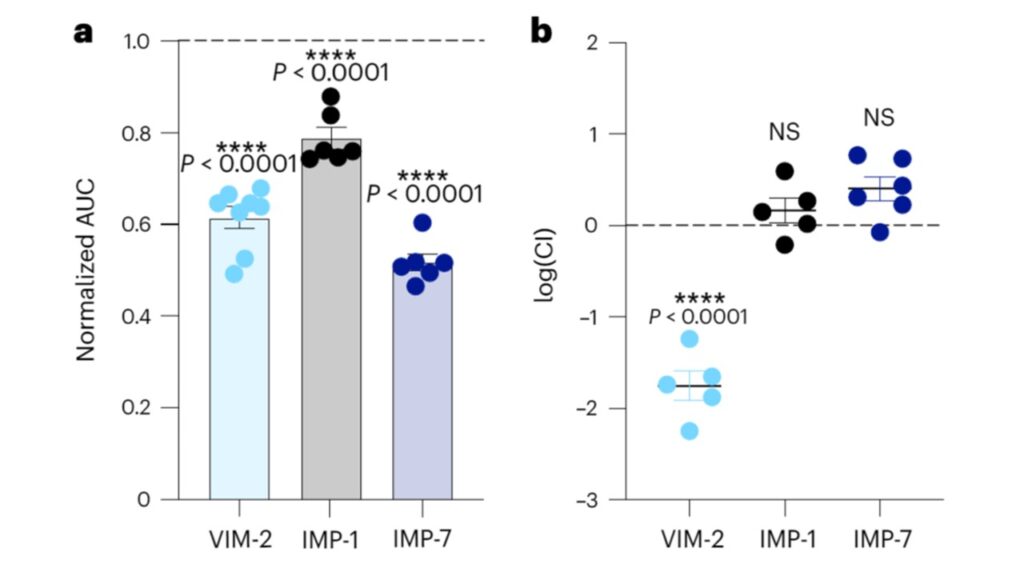
A study published in Nature Microbiology sheds light on the effects of zinc limitation on resistant bacterial strains. Researchers discovered that depriving these pathogens of zinc significantly impaired their growth and diminished their resistance to antibiotics. This finding not only reveals an Achilles’ heel in resistant bacteria but also opens the door to innovative therapeutic approaches that exploit this vulnerability.
Eric Brown, PhD, a leading researcher at McMaster University, explains the importance of studying bacteria under nutrient-limited conditions. For decades, laboratory studies have focused on bacteria thriving in nutrient-rich environments, which do not accurately reflect the conditions bacteria face within a human host. Brown’s team challenged this paradigm by investigating how bacteria adapt to nutrient scarcity, particularly zinc deprivation, and found that this stress severely weakens resistant strains.
The Impact of Zinc Deprivation on Bacteria
The research demonstrates that bacteria exposed to zinc-depleted environments, such as those mimicking the human bloodstream, face significant physiological challenges. Without adequate zinc, critical bacterial enzymes lose their functionality, leaving the pathogens unable to sustain themselves or defend against antibiotics. The study’s findings also highlight the critical role of envelope stress response pathways in bacteria. These pathways, essential for maintaining cellular integrity under stressful conditions, become key targets when bacteria face zinc scarcity.
Innovative Therapeutic Strategies
The implications of this research extend far beyond the laboratory. By identifying the critical role of zinc in bacterial survival, scientists are exploring ways to develop therapies that inhibit zinc acquisition. For instance, researchers are investigating molecules that can sequester zinc or block bacterial uptake systems. Such strategies aim to create environments where bacteria are unable to access the zinc they need, thereby reducing their ability to resist antibiotic treatment.
Therapies targeting zinc dependency offer the potential to restore the efficacy of existing antibiotics. This approach is particularly appealing as it circumvents the lengthy and costly process of developing entirely new drugs. By weakening bacteria’s defenses, zinc-targeting therapies can enhance the effectiveness of antibiotics already in use, providing a double-pronged attack on resistant infections.
Challenges in Developing Zinc-Targeting Therapies
Despite the promise of this approach, several challenges remain. One significant concern is the specificity of zinc-targeting treatments. Zinc is also essential for human cells, meaning therapies must be carefully designed to selectively affect bacterial systems without disrupting zinc homeostasis in the host. Another challenge lies in the potential for bacteria to adapt to zinc-limiting conditions over time. This highlights the need for robust clinical testing and the development of combination therapies that incorporate zinc deprivation with traditional antibiotics.


Leave a Reply