New research published in Nature sheds light on the intricate workings of chimeric antigen receptor T cell (CAR T) therapies, offering insights into why these treatments are effective and how they improve with time. The study, conducted by scientists from the Children’s Hospital of Philadelphia (CHOP) and Stanford University School of Medicine, unveils the pivotal role of the FOXO1 protein in bolstering the action of CAR T cells. These findings, detailed in a paper titled “FOXO1 is a master regulator of memory programming in CAR T cells,” carry significant implications for enhancing the efficacy of CAR T therapies, which have emerged as potent weapons against lymphomas, leukemias, and various other cancers.
Problem of limited clinical remission
CAR T therapies have revolutionized cancer treatment, yet their effectiveness varies among patients, with fewer than 50% experiencing long-term remission. One of the obstacles to their success lies in the limited lifespan of CAR T cells within patients. However, previous studies have noted that patients achieving lasting remission harbor more durable CAR T cells. The latest research elucidates that the presence of the FOXO1 protein correlates with prolonged cell survival and enhanced functionality of CAR T cells.
Factors that influence T cell memory
Dr. Evan Weber, senior author of the study and an assistant professor of pediatrics at the University of Pennsylvania Perelman School of Medicine, emphasizes the significance of understanding factors that influence T cell memory, such as FOXO1. He notes, “By studying factors that drive memory in T cells, like FOXO1, we can enhance our understanding of why CAR T cells persist and work more effectively in some patients compared to others.”
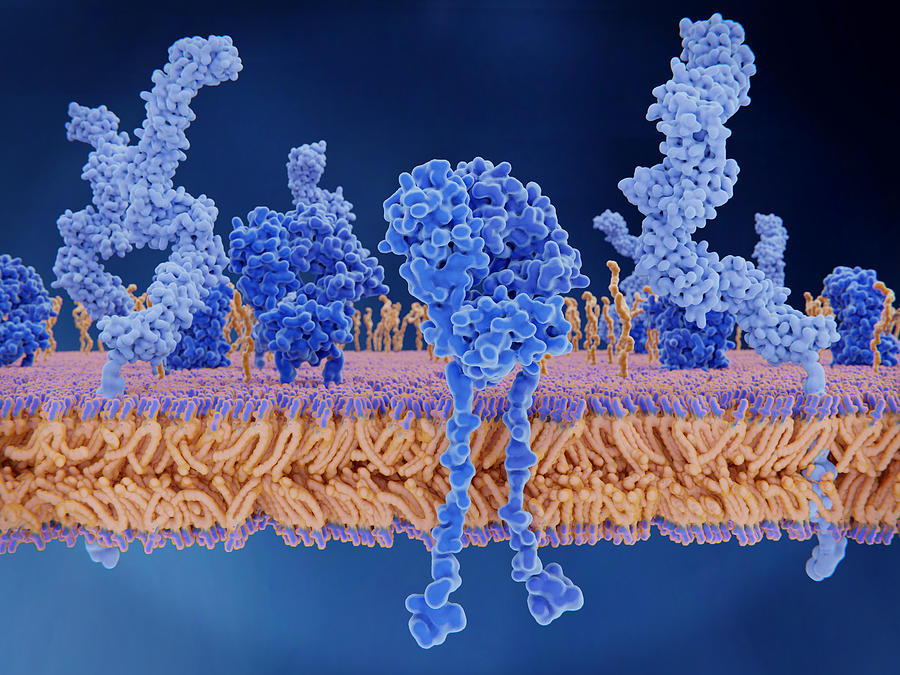
FOXO1, a protein known to activate genes associated with T cell memory, has predominantly been studied in mice, leaving its role in human T cells, especially CAR T cells, relatively unexplored. To bridge this gap, researchers employed CRISPR technology to eliminate FOXO1 in human CAR T cells. The results were striking: without FOXO1, CAR T cells lost their ability to form robust memory cells and combat cancer effectively in animal models.
Conversely, when FOXO1 expression was heightened in CAR T cells, a cascade of positive outcomes ensued. Not only were memory genes activated, but the T cells also exhibited improved persistence and enhanced anti-cancer activity. Importantly, manipulating other memory-promoting factors did not yield similar benefits, underscoring the unique role of FOXO1 in bolstering CAR T cell function.
Future prospectives
Dr. Weber underscores the potential impact of these findings on CAR T cell therapy design, stating, “These findings may help improve the design of CAR T cell therapies and potentially benefit a wider range of patients.” Collaborative efforts are underway to identify additional proteins akin to FOXO1 that could further augment the durability and therapeutic efficacy of CAR T cells.
The study’s findings underscore the potential of memory reprogramming as a strategy to optimize therapeutic T cell states. Despite the complexities involved in CAR T cell therapy, elucidating the role of FOXO1 opens new avenues for enhancing treatment efficacy and prolonging patient remission. Ongoing research efforts aim to capitalize on these insights to refine CAR T cell therapies and broaden their applicability across a spectrum of cancer types.